A daring dive into the gut of innovation at **Cincinnati Children’s Hospital Medical Center, where the absurd notion of rectal ventilation is inching toward real-world rescue.
What if your body could bypass your lungs altogether? That wild idea isn’t just sci-fi anymore—thanks to research from Cincinnati Children’s, it’s edging into reality.
From IgNobel to “I Might Be Saved”
Back in 2024, a research concept won the coveted (and comedic) Ig Nobel Prize for “butt-breathing”. Yes, you read that right. The idea: deliver oxygen into the bloodstream not through the lungs, but via a super-oxygen-rich liquid introduced in the colon (a procedure the team calls “enteral ventilation”). Research Horizons
Fast forward to October 20, 2025: the team published the first human safety study in the journal Med. It’s still early days, but the shift from absurd to plausible is real. Research Horizons
of Cincinnati Children’s leads the pioneering “butt-breathing” research, turning an Ig Nobel idea into a potential life-saving therapy for patients who can’t breathe on their own.
What the Research Shows
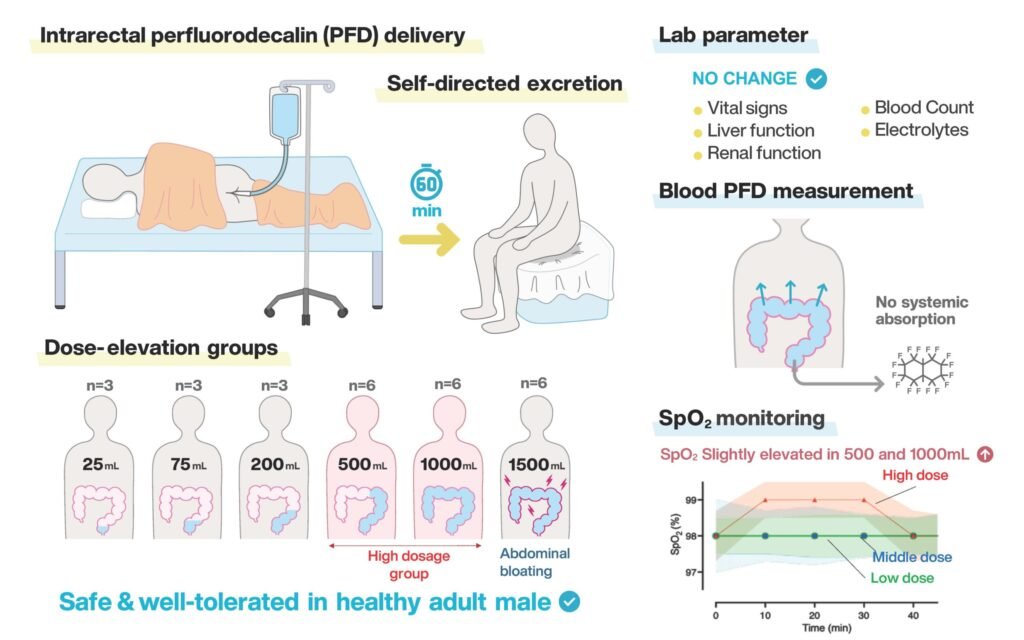
- Twenty-seven healthy men in Japan tested this method, holding intrarectal volumes of up to 1,500 ml of non-oxygenated perfluorodecalin (a liquid known to dissolve oxygen) for 60 minutes. Twenty of them completed the full test. Research Horizons
- At the largest volumes, participants experienced bloating and discomfort, but no serious adverse events. Safety milestone ✅. Research Horizons
- Important caveat: This study was about tolerability, not efficacy. They haven’t yet shown that the method delivers enough oxygen into the bloodstream to replace or supplement lungs. Research Horizons

- The inspiration? A bottom-dwelling fish called a loach that swallows air and absorbs oxygen through its gut when oxygen is scarce. Nature’s weirdness strikes again. Research Horizons
- The idea also builds on previous research involving perfluorocarbon liquids and even references the 1989 movie The Abyss (yes, that liquid-breathing rat scene) where a rat breathes liquid in a sci-fi flick—art imitating science, or maybe science imitating art. Research Horizons
Why It Matters
In critical care situations, severe lung injury, blocked airways, newborns with underdeveloped lungs … a method to deliver oxygen that doesn’t rely on the lungs could transform outcomes. The Cincinnati Children’s team believes this could become a low-tech, widely deployable tool when traditional ventilation fails. Research Horizons
Given that lung diseases are leading causes of death and disability, imagining a backup system for the backup system is no joke.
⏭️ Next Steps: From “It’s Safe” to “It Works”
Here’s where the journey goes next:
- Switch to oxygenated perfluorodecalin (or a similar oxygen-rich liquid) to measure how much oxygen actually enters the bloodstream and how long the effect lasts.
- Define the optimal liquid volume, dosage duration, and conditions (e.g., adult vs. neonatal use, injured lung vs. healthy lung).
- Explore use in vulnerable populations: newborns, patients with lung failure, or settings without advanced ventilation equipment. The study mentions an expansion into newborn care as a goal. Research Horizons
- Fundraising and regulatory pathways: the research team has launched a company, EVA Therapeutics, to move this into broader trials, but pace depends on funding. Research Horizons
- Address practical and ethical challenges: safety in more vulnerable populations, long-term effects of intrarectal oxygen delivery, potential complications, and public perception (yes, that “butt-breathing” headline is hard to shed).
🧪 A Serious Science, With a Humorous Label

Don’t let the giggle-factor fool you. The label “butt-breathing” may bring chuckles, but the science is serious, and the stakes are high. The researchers at Cincinnati Children’s aren’t just chasing novelty. They’re chasing survival.
Innovation often looks absurd until someone makes it real. This may be one of those cases.
What’s Next for This Science Project
- A Phase II trial: test efficacy (oxygen delivery, clinical endpoints) in a patient population, not healthy volunteers.
- Device/formulation refinement: what’s the optimal liquid, delivery system, monitoring equipment, safety protocols.
- Regulatory and ethical review: enteral ventilation will need clearance from medical regulators, ethical studies in humans, and defined guidelines.
- Scaling for clinical use: if it works, how to implement in emergency rooms, neonatal care units, resource-limited settings.
- Long-term safety tracking: watch for colonic or systemic side-effects, interactions with other therapies, durability of benefit.
In short: what began as a cheeky idea is now inching toward life-saving seriousness. At Cincinnati Children’s, science is boldly going where no therapist has gone before, right through your colon (with permission, of course). Stay tuned. This is one of those weird pathways science takes that just might matter a lot.