A phlebotomist at Mat-Su Regional Medical Center provides a lab draw for a patient, highlighting the behind-the-scenes care that supports diagnosis and treatment every day in the Mat-Su Valley. Local hospitals and clinical staff like these are among the providers that could benefit from Alaska’s Rural Health Transformation Program as the state invests in workforce stability, modernized care, and improved access to health services close to home.
Photo credit: Mat-Su Regional Medical Center / Facebook
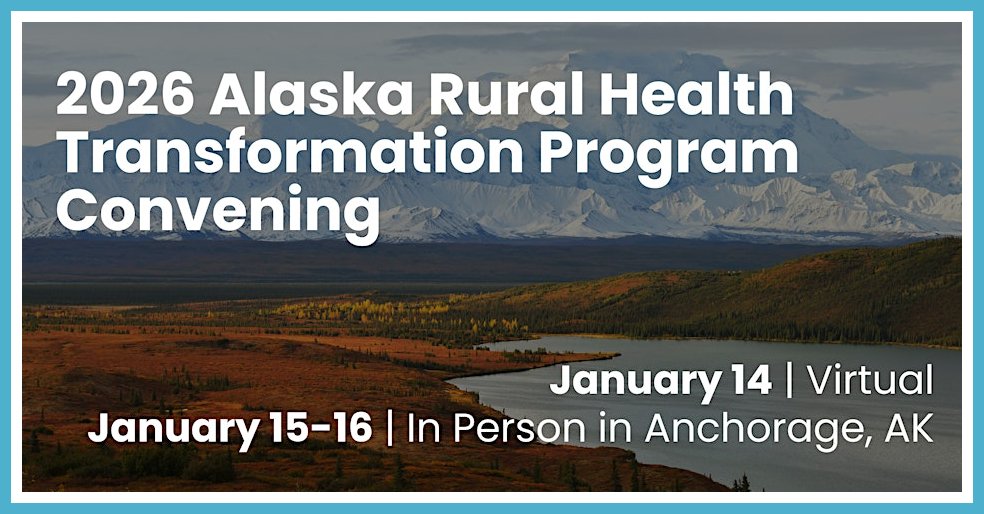
A major federal investment is headed toward Alaska’s health care system, and while the effects will not appear overnight, the decisions made over the next year will shape how care is delivered across the state for a generation. The Centers for Medicare and Medicaid Services has awarded Alaska about $272 million for 2026 under the new Rural Health Transformation Program, part of a $50 billion national effort designed to strengthen health care in rural and frontier communities.
For Alaska, this funding arrives with unusual flexibility. Rather than directing the money to a single hospital or program, the state has proposed a broad, statewide approach that treats Alaska as one connected health system. The goal is to strengthen access to care close to home, stabilize a strained workforce, modernize facilities and technology, and support new ways of paying for care that reward better outcomes instead of higher volume.
What matters most for residents is that this funding does not automatically flow to clinics or hospitals. Much of the money will be distributed through competitive sub grants beginning in 2026. That means local health providers, Tribal health organizations, nonprofits, emergency services, training programs, and community groups will decide where the dollars land by applying for them. Public participation and local advocacy will influence which priorities rise to the top.

Photo credit: Alaska Headline Living © December 2025
The Mat-Su Valley sits at an important crossroads in this process. While federal agencies do not always classify the borough as rural because of its connection to the Anchorage metropolitan area, Alaska’s plan does not rely on rigid geographic labels. Health systems in Wasilla and Palmer serve residents from remote roadless areas, absorb provider shortages, and face many of the same access challenges as communities off the road system. Because the program focuses on outcomes and regional impact, projects based in the Mat-Su Valley that strengthen rural care or support statewide access can still qualify for funding.
Over time, that could mean expanded telehealth services, more behavioral health and maternal care options closer to home, better coordination between emergency responders and hospitals, and stronger incentives to recruit and retain health workers who want to live and work in the Valley. It could also support training pipelines that help local students enter health care careers without leaving the region, keeping providers rooted in the community.

Photo credit: Turnagain Telehealth
It is also important to be clear about what this program does not do. It does not provide direct payments to individuals or immediately reduce medical bills. The changes people feel will come through systems that work better, providers who stay longer, and services that reduce the need for long and costly travel. The law that created this program also includes broader changes to federal health spending, meaning this investment strengthens access but does not replace every benefit that may be reduced elsewhere.
This plan is not finished. Alaska’s proposal outlines priorities, not final projects. The Department of Health will hold public meetings, release guidance, and open application periods over the coming year. Residents who pay attention now, speak up, and encourage local organizations to apply can influence what services exist five and ten years from now. This funding will shape Alaska’s health care future, and communities that engage early will have the strongest voice in how it is used.
Get More Information and Get Involved
Readers who want to follow Alaska’s Rural Health Transformation Program or take part in upcoming discussions can start with the State of Alaska Department of Health’s program page which includes background information, updates, and registration links for public meetings and events. Questions, comments, or ideas about how the funding should be used can be emailed directly to DOH.RHTF@alaska.gov. The Alaska Department of Health can also be reached by phone at 907-269-7800 or by email at doh.info@alaska.gov.
Those interested in rural health policy, workforce development, or community engagement can contact the Alaska State Office of Rural Health at 907-269-3445 or by email at doh.rchs.info@alaska.gov. Information about the national Rural Health Transformation Program is available from the Centers for Medicare and Medicaid Services and federal program questions can be sent to MAHARural@cms.hhs.gov.
For help with Medicaid related questions or referrals to state health resources, the Alaska Medicaid office can be reached toll free at 800-780-9972 or locally at 907-465-3030. Workforce and training information is also available through the Alaska Center for Rural Health and Health Workforce at the University of Alaska Anchorage at 907-786-6591 or uaa_ahec@alaska.edu.